Macular degeneration is an age-related eye disease that causes loss of central vision and typically comes in two forms known as dry macular degeneration and wet macular degeneration. If you are over the age of sixty years old and have not had a routine eye exam it is highly suggested that you schedule an eye exam to look for early signs of this degenerative eye disease.
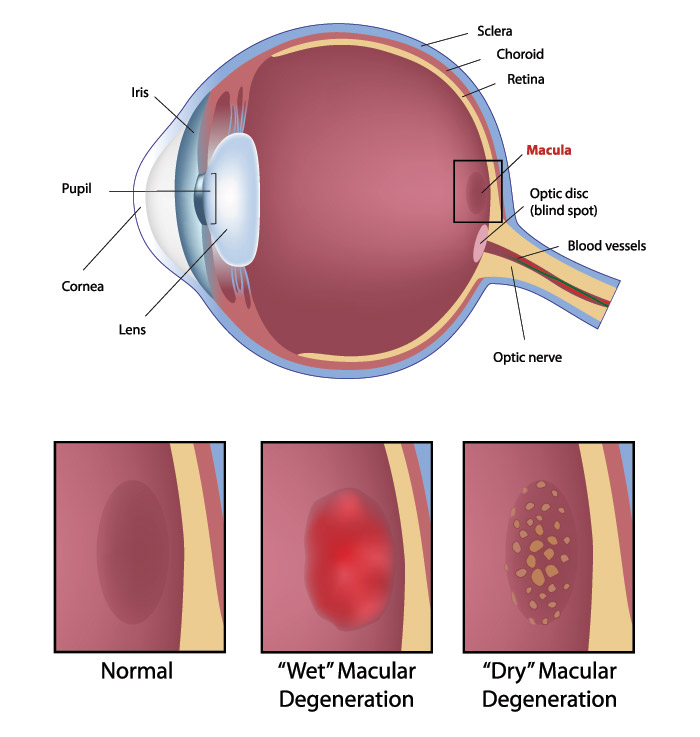
Macular Degeneration Diagram
- “Dry” form — the most common form usually progresses slowly and causes central vision loss.
- “Wet” form — rare, and more severe. May progress rapidly causing significant central vision loss.
Dry Macular Degeneration
The most common type of macular degeneration is the dry form of this disease, in fact, it affects about 90% of the cases seen by ophthalmologists. When you have this type, there are deposits, called drusen, under the retina, or degeneration of the layers under the retina (atrophy) with loss of photoreceptor function. Vision can range from minimal changes with the presence of drusen to severe loss with advanced atrophy. Dry macular degeneration can sometimes progress to wet AMD. There is no treatment for dry type of AMD, but prevention of progression to wet AMD is possible with a healthy diet antioxidant vitamins.
Wet Macular Degeneration
Wet Macular Degeneration refers to the presence of fluid or blood under the macula due to the formation of abnormal blood vessels under the retina (choroidal neovascularization). With wet AMD, vision can rapidly decline and it is this type that is responsible for severe vision loss.
Early detection and treatment are critical for preventing further loss of vision. Unfortunately, the disease is a chronic problem with a high rate of recurrence, and patients generally require multiple treatments over time. Fortunately, new treatment modalities are improving our ability to preserve vision for longer periods of time.
Detection of Macular Degeneration
The eye care team at The Regional Eye Center might have reason to think if you are over the age of 60 and have central vision loss that macular degeneration may have set in. In order to check for signs of this disease, our eye doctors will dilate your pupils in order to view the back of the eye better.
Listed below are some of the diagnostic tests that will be conducted:
- Visual acuity test – This eye chart test measures how well you see at various distances.
- Dilated eye exam – Drops are placed in your eyes to widen, or dilate, the pupils. Your eye care professional uses a special magnifying lens to examine your retina and optic nerve for signs of AMD and other eye problems. After the exam, your close-up vision may remain blurred for several hours.
- Tonometry – An instrument measures the pressure inside the eye. Numbing drops may be applied to your eye for this test.
Macular Degeneration FACTS
- Currently affects more than 10 million Americans.
- 2 types of macular degeneration (wet and dry).
- “Wet Macular Degeneration” is responsible for (90%) vision loss.
- The average age of detection is in the 70’s.
- Damage cannot be reversed.
- High myopia (nearsightedness) can lead to macular degeneration.
Macular Degeneration Treatment
The treatment of wet AMD has evolved over the last 20 years. The treatment options include laser, photodynamic therapy with or without injection of steroid into the eye, and injections of anti-VEGF drugs (Macugen®, Avastin, or Lucentis™) into the eye.
Laser
In the 1980s and up until the advent of photodynamic therapy, a thermal laser was used to destroy the abnormal new blood vessel complex. This technique was better than no treatment at all but patients were left with an immediate decrease in vision and a dark spot in their vision when treated with laser. Nowadays, a laser is used only for those lesions that are located away from the center of the macula or around the optic nerve.
Visudyne Treatment / Photodynamic Therapy (PDT)
This treatment involves an intravenous infusion of a light-sensitive drug (Visudyne) followed by directing a non-thermal laser beam to the abnormal blood vessel complex. Visudyne preferentially binds to components of the abnormal blood vessels and the “cold” laser light photoactivates the drug and causes these vessels to shut down. Recurrences do occur following this treatment, and the average number of treatments is 3 in the 1st year, 2 in the 2nd year, and 1 in the 3rd year after diagnosis of wet AMD. Injection of a steroid called kenalog is typically used in conjunction with PDT.
Anti-VEGF Drugs
In wet AMD, there is an upregulation of vascular endothelial growth factor (VEGF). Anti-VEGF drugs block VEGF from binding to receptors on blood vessels and cause regression of the abnormal new blood vessel complex. Currently, there are 3 such drugs available.
Pegaptanib (Macugen®):
This is the first FDA-approved anti-VEGF drug and has shown to be efficacious in preventing further loss of vision in patients with wet AMD. This drug is injected in the eye every 6 weeks. In studies comparing this treatment to no treatment at all, 70% of treated eyes versus 55% of untreated eyes lost less than 3 lines of vision at 1 year. There is a 15% treatment benefit, and treated eyes lose less vision over 2 years than untreated eyes.
Lucentis™
This drug was approved by the FDA in June 2006 for the treatment of wet AMD. It is an antibody fragment that binds VEGF. This drug is injected into the eye every 4 weeks. In studies comparing treatment to no treatment, 94.5% of treated eyes versus 62.2% of untreated eyes lost less than 3 lines of vision at 1 year. Furthermore, 25 to 33% of patients gained vision with treatment.
Avastin®
This drug is FDA-approved for the treatment of colon cancer. It is a full-length antibody against VEGF and is a bigger molecule compared to Lucentis, which is a fragment antibody. It has been successfully used off-label for the treatment of wet AMD with no reported safety concerns.
Treatment involves injections every 4 weeks until the abnormal blood vessel complex resolves and the patient is then followed periodically to watch for recurrences. The resolution of the abnormal blood vessel complex after 1 or 2 treatments has been shown in retrospective studies.